What Services Does Palliative Care Provide?
Palliative care has been a board-certified medical specialty since 2006 in the US, but the practice of comfort-focused care has been around for centuries. Palliative treatment grew out of the hospice movement.
Today, 80 percent of hospitals with 300 or more beds offer a palliative specialist or palliative team that works with the patient’s other physicians to address the physical, social and spiritual distress of serious illness and its treatment and care choices.
What Is Palliative Care?
Palliative care is care that provides relief from symptoms resulting from disease or injury.
In comparison to curative care, which is meant to cure a disease, palliative care is meant to make the patient more comfortable. The definition of palliative care is "to make a disease or its symptoms less severe or unpleasant without removing the cause." Palliative care will lessen or "palliate" the symptoms and improve your quality of life.
Is Palliative Care the Same as Hospice Care?
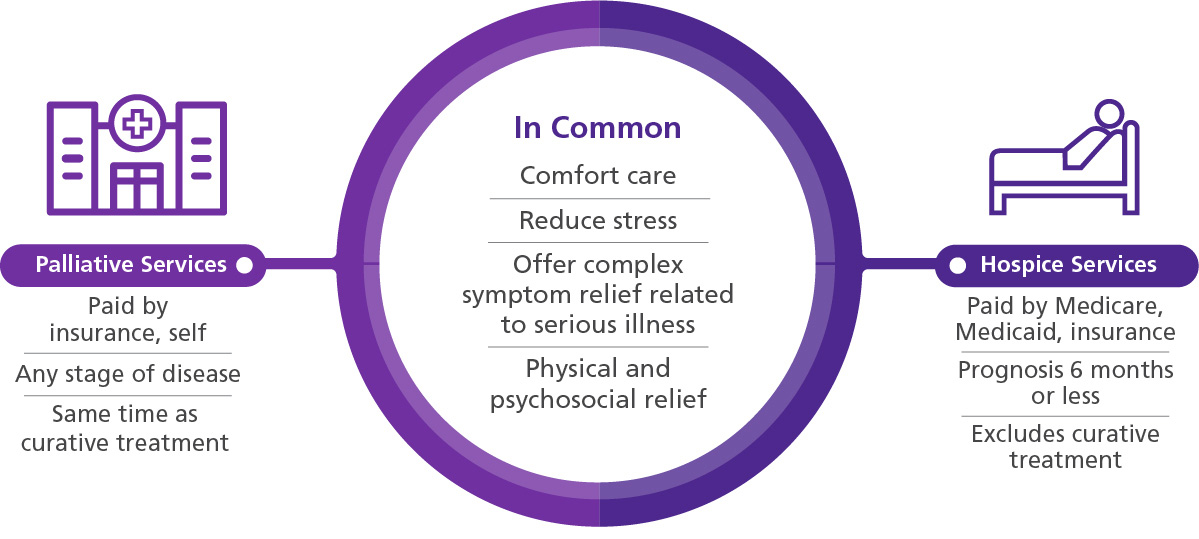
No. While palliative and hospice care both address symptoms, hospice is appropriate only in the last six months of life, as estimated by the patient’s physician. Hospice is offered in place of curative treatment, whereas the comfort of palliative care is available at any time in a patient’s disease, from diagnosis and throughout curative treatments.
Learn more about the differences between palliative care and hospice care >
Generally, palliative medicine is discussed in the context of serious illness: chronic, progressive pulmonary disorders; renal disease; chronic heart failure; HIV/AIDS; progressive neurological conditioners; cancer; etc. It focuses upon the nature of treatment and the possible and impossible outcomes of therapy options.
The intention of palliative care is to provide information to the patient and family so they can determine their goals and desired outcomes — thus the term “Goals of Care Discussion.”
What Are the Goals of Palliative Care?
Palliative care goals include:
- Aligning treatment outcomes with the patient’s values and preferences
- Improving quality of life for both the patient and the family
- Minimizing pain and discomfort
- Alleviating emotional distress, anxiety, or depression
- Assisting with safety, mobility, and equipment
- Spiritual counseling
- Empowering patients and caregivers to make decisions that are right for them
Who Is on the Palliative Care Team?
Palliative care is most often provided by a team of professionals very similar to an interdisciplinary hospice team. Clinical evaluation and care discussions are usually provided by physicians, nurse practitioners, and RNs. At times, social workers and chaplains are also involved.
What Are the Benefits of Palliative Care?
Palliative care provides relief in a variety of ways. Physical symptoms such as pain, fatigue, loss of appetite, nausea/vomiting and sleep loss can all be mitigated with palliative approaches, whether through drugs, nutrition, deep breathing, or acupuncture.
For patients and families struggling to cope with a serious diagnosis, palliative care can address depression, anxiety, and fear by employing counseling, support groups, family meetings, and the like.
What Is Included in Palliative Care?
Palliative care begins with a conversation to determine the patient’s symptoms, needs, and any medications that may provide relief. For some patients, ending medications that cause uncomfortable side effects is offered as a palliative option.

The patient’s needs also may be met using approaches that don’t rely on medication, such as specialized nutrition or breathing exercises. For additional relief, the palliative care team can introduce complementary therapies to address specific symptoms.
The specifics of palliative care vary from case to case, as treatments are intended to address a patient’s unique needs and tolerance for discomfort.
The palliative care team routinely communicates with the patient to determine the intensity of their pain and other symptoms. Based on that information, they assess appropriate treatment options together.
When a patient is unable to communicate or otherwise unable to self-report pain or other bothersome symptoms, the care team relies on pain assessment tools and clinical judgment to facilitate symptom relief.
How Long Can You Be in Palliative Care?
Palliative care can occur at any point in life, for any duration, and it can occur in conjunction with curative care. Hospice care, which includes palliative care, is designed to provide comfort and dignity in the last six months of a patient’s life.
Research suggests that earlier initiation of palliative care has a positive impact on patient and family satisfaction with the care they receive, patient perceptions of pain, and even patient survival rates. A hospice patient who chooses to discontinue hospice services can continue to receive palliative care.
Talking to Your Healthcare Providers About Palliative Care
For patients and families facing worries beyond the illness itself, a member of the VITAS palliative care team can assist with questions and help find resources to address financial, legal, employment, transportation, and housing issues. And whether your faith is your anchor, or it feels like it has abandoned you—or even if you have no religious background at all—palliative care can address any spiritual questions in light of your culture and traditions.
Palliative care clinicians are trained above all to listen to patients’ and families’ needs, goals, concerns, and questions. They take patients’ feelings and subjective experience of pain seriously, and skillfully lead conversations that can uncover unresolved issues to inform a comprehensive, patient-centered care plan.
Palliative care has been proven effective in improving quality of life. When your symptoms are controlled, and you feel like someone is there to listen, you feel better and live better. Palliative consults result in lower healthcare costs, because they may help you to feel well enough to choose to stay out of the hospital and decline tests or treatments that don’t align with your goals.
How Does VITAS Approach Palliative Care?
At VITAS, palliative care begins with a plan uniquely tailored by an interdisciplinary team to meet the needs of the patient. The team can work with newly diagnosed patients and those struggling with the effects or after-effects of curative therapies. Some members of the palliative team may be board certified in hospice and palliative medicine; others range from chaplains to social workers.
A palliative consult with the patient provides timely and specific information that helps the patient and family understand what palliative medicine brings to the table and helps physicians and the rest of the interdisciplinary team provide the most appropriate care.
If the patient’s symptoms escalate and can no longer be managed by routine palliative care, VITAS is available 24/7 to transition the patient to a higher level of care with round-the-clock support from a crisis nurse until symptoms are back under control. If symptoms are especially aggressive, VITAS can transfer the patient to an inpatient hospice unit for intensive symptom management until they’re ready to return home.